Almost six people a day die from drug overdoses in Australia.
In its 2018 overdose report[1] the Penington Institute revealed that more than 1,700 drug related deaths in Australia were accidental, and most of these involved prescription medications.
Now Victoria has started to roll out a ground-breaking cloud-based real-time prescription monitoring system to medical practitioners and pharmacists that will perform a key role in helping to reduce the risk for many of these avoidable deaths. To set this in context, in 2017, 414 Victorians died from this problem, more than the State’s road toll.
Called SafeScript, the new system monitors the prescription and dispensing of all controlled (Schedule 8) medicines such as morphine and oxycodone, as well as other higher risk medicines including codeine and diazepam. Coupled with an education initiative for consumers and practitioners, the Victorian Department Health and Human Services (DHHS), is confident that its $30 million investment will rein in accidental deaths by overdose across the State and set a benchmark for other States and Territories that do not currently have such a system.
As Matthew McCrone, director of real time prescription monitoring implementation for DHHS, explains; “The problem is that too many people are dying from prescription medicines, from overdose. That number is ever-growing. We have had things in place for a very long time in Victoria, to regulate these high-risk medicines; clearly, we needed to transform how we go about doing this, in order to prevent these deaths occurring. So, preventing deaths from prescription drug overdose is why we’re doing this. And the way to get there is to help doctors and pharmacists make more informed clinical decisions and thus facilitate safer prescribing and dispensing of these high-risk medicines.”
SafeScript connects to pharmacy and GP software to streamline workflow. “It is, ultimately, about making sure that the clinician has information in front of him or her, at the point that they’re needing to make a decision about whether to prescribe a particular medicine or dispense it. So, SafeScript provides them that information in as seamless a way as possible. Equally important – and, this is the other thing that we need to deliver – is that the clinician knows what to do next.
“If they have information in front of them that they wouldn’t have otherwise had – for example, that that patient is seeing other doctors or is on other medicines, which means the medicine they were considering is even more risky – the clinician needs to know what they’re going to do next. How are they going to support that patient so that things work out safely for them? That’s why the workforce training that we’re delivering is part of the project. It’s so utterly crucial to the overall objectives of the project.”
[1] http://www.penington.org.au/australias-annual-overdose-report-2018/
“The problem is that too many people are dying from prescription medicines, from overdose. That number is ever-growing. We have had things in place for a very long time in Victoria, to regulate these high-risk medicines; clearly, we needed to transform how we go about doing this, in order to prevent these deaths occurring. So, preventing deaths from prescription drug overdose is why we’re doing this. And the way to get there is to help doctors and pharmacists make more informed clinical decisions and thus facilitate safer prescribing and dispensing of these high-risk medicines”. – Matthew McCrone, director of real time prescription monitoring implementation for DHHS
Real time alerts
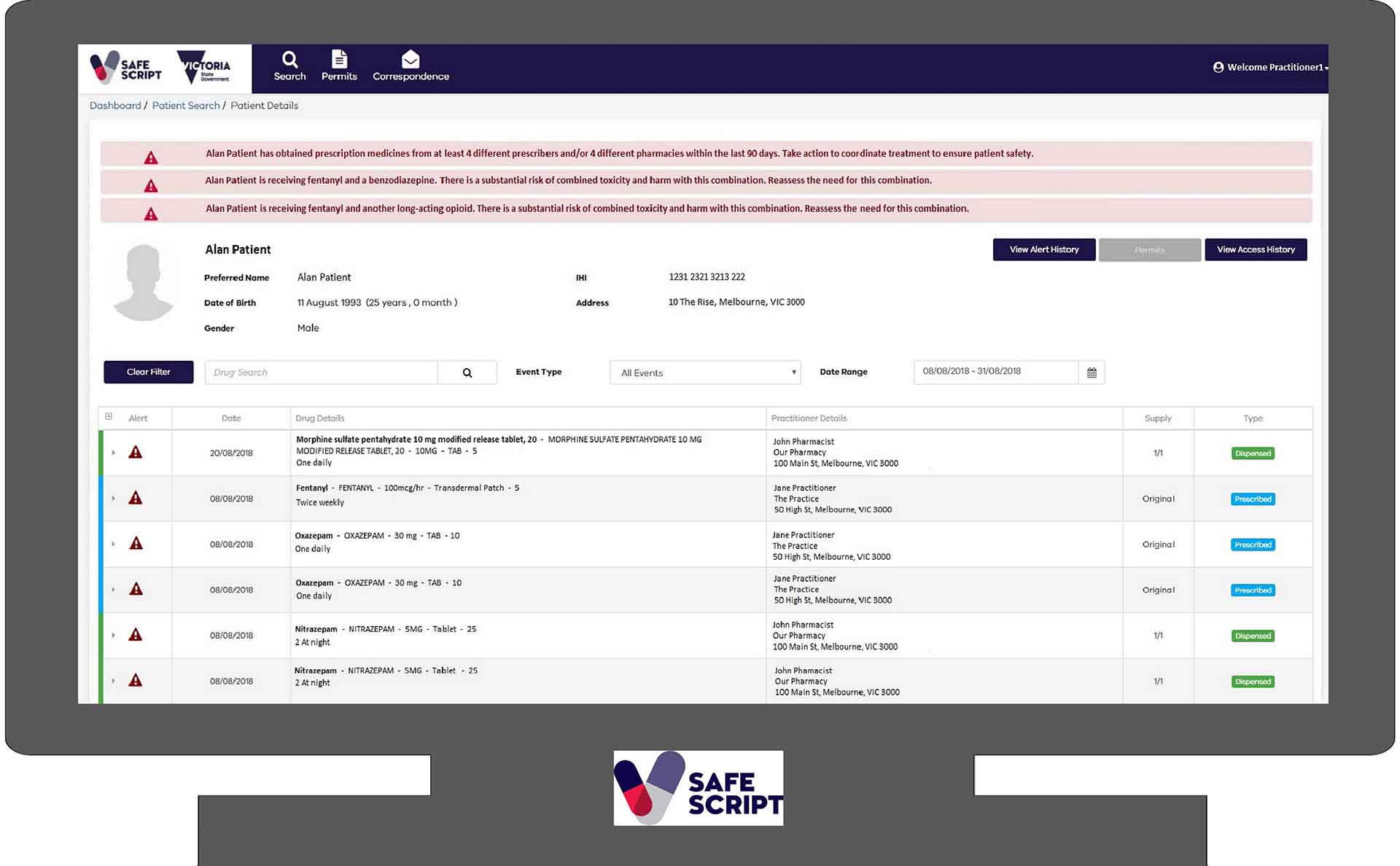
Developed by specialist pharmacy solution provider Fred IT Group, SafeScript offers doctors and pharmacists a real time alerting capability. If the system detects that a patient has gone to multiple providers for the same medicine over a short period of time, or they are using a risky combination of medicines that elevates the risk of overdose, it will automatically raise an alert.
A staged roll out is underway, with the first implementation live across the Western Victoria Primary Health Network since the start of October 2018, ahead of a statewide roll out in April 2019. From April 2020, every medical practitioner and pharmacist in Victoria will need to access SafeScript before they dispense or prescribe the monitored medicines.
Being based on Microsoft’s trusted Azure cloud ensures the security needed by such a sensitive application, but also provides the scalability and reach which will be required as the solution is rolled out across Victoria, and the flexibility to monitor new medications as required. System performance and resilience is also critical; one of DHHS’ technical requirements was that the system needed capacity to support the potential use by all Victoria doctors and pharmacists (more than 30,000 clinicians) at any time.
Paul Naismith, CEO of Fred IT Group (Fred), who is also a pharmacist, says that the system has been designed so that the information is presented to the clinician or pharmacist in less than three seconds. “We couldn’t have done this without the maturity of Azure.”
Using Azure Event Hub, Stream Analytics, WebJobs and Enterprise Service Bus, the solution ingests real time prescription and dispensing data captured via the electronic transfer of prescriptions through eRx Script Exchange and MediSecure, processing the data to be stored in Azure SQL. Data insights are pushed into PowerBI for further analysis and reporting.
Azure Active Directory is used to control access, ensuring only authorised personnel can use SafeScript. Working with the Australian Health Practitioner Registration Authority, which is responsible for registering medical and other health practitioners, Fred has created profiles for eligible practitioners and invited them to register for an account with SafeScript. Once registered, Azure Active Directory along with multi-factor authentication manages access to the system.
According to Naismith, this is one of the largest deployments of multi-factor authentication in the Australian health sector to date.
Web apps provide access to SafeScript portals to authorised users, ensuring a better performance regardless of bandwidth – which is important for rural or regional practitioner access.
Intelligent insight
As Naismith explains; “Before SafeScript, you could only see what you prescribed or dispensed at your clinic or pharmacy. Now you can actually see if your patient has visited other doctors or pharmacies for the same medication, so you know who their doctor is, you can talk to the doctor, you can get the information you need, and just having those alerts to know if there is a problem. And it’s not necessarily anything the patient is doing, there’s a number of different things that are being looked at in terms of SafeScript: are they on a safe dose? Are they on multiple medications that may cause issues? Is there a combination of toxicity there? Things that you don’t necessarily see if they go to a different pharmacy or a different doctor.”
Lena Belfield, DHHS project director explains that the technology foundations are critical – but so too is the supporting framework. “The IT tool that we developed, leveraging the Microsoft Azure platform, is an enabler, but there’s a whole host of other work streams in the project around the IT, including workforce and consumer support, GP and pharmacist training that we need to deploy – basically, to support quite a large-scale change in clinical practice. Our underlying purpose is to change the culture of prescribing and dispensing high-risk medicines by doctors and pharmacists.”
DHHS chief information officer Dr Steve Hodgkinson says; “The project is a further example of our successful Platform+Agile approach. We have leveraged modern cloud services platforms and existing systems to the fullest extent possible and used agile, iterative, development to deliver early results and to enable the system to be refined based on user feedback. The approach has delivered exceptional results – and now provides a scalable, robust and flexible platform for expansion to become a national system.”
Working with Microsoft partner CNI, DHHS developed a hosting framework in Azure to manage security, event management and disaster recovery, which enables rapid and repeatable, highly secure application.
Since the go-live of Stage One, Fred is now working on fortnightly sprints, with regular releases at the end of every fortnight. Hot fixes and priority items can be released earlier with no impact to the end user.
Already there are signs of the impact that SafeScript will have, says McCrone; “Pharmacists that have come to learn that a particular patient had got X number of this medication and Y number of that medication in a period of 90 days, or a doctor who has been treating a patient with methadone for opioid addiction for some years and has realised that patient is also going to other doctors and is getting other opiate medication.”
There are other equally compelling impacts in terms of heading off opioid addiction. Clinicians have told McCrone that had such a system been in place when someone visited them after being in a car accident, or for relief from lower back pain; “The clinicians would have had the information in front of them, and they never would have ended up in the place that they did end up. That’s pretty compelling, for us.”
It’s pretty compelling for all Australians.
If you or someone you care about has a problem with prescription medicines, the SafeScript Pharmaceutical Helpline may assist with counselling, information and referral to treatment and support services.
The SafeScript Pharmaceutical Helpline is a free and confidential 24-hour telephone counselling service: 1800 737 233