Doctors help build smartphone app, leverage cloud to monitor COVID-19 patients
One of the most pressing problems for countries all around the world has been finding a way to avoid health services being totally swamped by COVID-19.
The most valuable resource in every hospital is the human factor in delivering patient care, in terms of doctors, nurses, and allied health staff encompassed with the need for inpatient beds The ability to safely monitor isolated patients in the community, thus keeping people out of hospital, ensures those resources remain available for the most critical patients.
It was a challenge for South Eastern Sydney Local Health District (SESLHD) which operates a number of hospitals including Prince of Wales (POWH), Sutherland and St George Hospitals and provides health services to almost a million people.
When COVID-19 struck, Dr Sze-Yuan Ooi – a cardiologist at POWH – realised that a system he had been working on to provide remote monitoring and support to cardiac patients could possibly be repurposed to monitor COVID-19 patients. Besides his role as a doctor, Ooi is a conjoint senior lecturer at UNSW Sydney which played a key role in the development of the TeleClinical Care – Cardiac system.
Working with Professor Nigel Lovell, head of the Graduate School of Biomedical Engineering at UNSW, Ooi helped design the remote monitoring system which uses smartphone technology and sensors to transition patients from hospital to home while continuing to monitor them, facilitating self-care and reducing unnecessary re-hospitalisations.
That project recently secured a grant of almost $2 million from NSW Health to run a large multisite study across multiple hospitals in NSW.
But Ooi and Lovell pivoted their attention when; “COVID struck and it seemed to us that the pressing problem globally is that when health systems are inundated community monitoring is unsustainable.”
While TeleClinical Care – Cardiac solution had been developed to provide patient monitoring, it hadn’t been designed to scale to be able to deal with thousands, maybe tens of thousands of patients. Any COVID-19 monitoring system developed from its scaffold would need to be highly scalable, reliable and secure.
Lovell and his team at UNSW have been working with Ooi on the cardiac patient system as well as other telehealth platforms to support people with Parkinson’s disease, respiratory conditions and patients recovering from strokes. They have also been working with the relevant clinicians and Virtual Care Centre being established at POWH, which is designed to be a hub for healthcare innovations that can provide in-community support to patients – but also act as the conduit to other healthcare services when required.
For the COVID monitoring system it was clear that scale and speed were critical. Working with Microsoft Fast Track for Azure, Lovell and his team – supported by the IT team at SESLHD – were able to transition the system they had developed out of an on-premise data centre into Azure in a week. They then tested the system with about 100 users to fine–tune it and had a system ready to go in around three weeks.
Patient monitoring
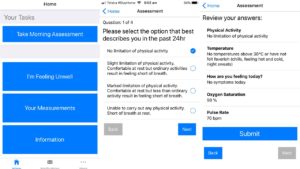
The COVID-19 monitoring platform is a Django application now running on Azure. COVID patients who are referred by the fever clinic download a smartphone app, are enrolled in the system the POWH Remote Monitoring Solution team and have a pulse oximeter delivered to their home, where they remain isolated while being COVID positive.
The system collects information about the patient, their other health issues and vital signs. Once enrolled, patients fill in a questionnaire twice a day prompted by the app.
The first question in the morning asks them about symptoms, predominantly whether they’re febrile or feel hot and if they have any symptoms of breathlessness and what they can and can’t do without getting breathless.
Patients also enter their pulse rate and oxygen saturation levels using the oximeter. All that data is then loaded to the app portal, analysed in Azure, and if it exceeds certain thresholds set by the clinician, further action is triggered.
Joshua Head, a software engineer at UNSW adds: “For example, Sze–Yuan says, ‘Oh, I want an alert every time X happens.’ And then we write the code that does that alert and then triages it to the correct person.”
According to Ooi;
The TeleClinical Care COVID solution allows us to remotely monitor patients’ pulse rate and oxygen saturations. This allows early detection of clinical deterioration. We know that even when patients with COVID-19 have severe pneumonia and very low oxygen levels in the blood they can be almost asymptomatic.
Having an early warning of any deterioration can allow health professionals to step in quickly and potentially rein in the risk of respiratory distress and further deterioration.
Bringing a new hospital onto the platform is relatively straightforward says Head. “We used Azure pipelines to actually deploy a complete automated environment. It takes us 40 minutes to deploy into a new Azure subscription and then they’re up and running.”
Importantly, the system is scalable as the inbuilt analytics automatically triages patients according to health risk. According to Lovell; “The backend clinician portal immediately re-stratifies people and generates red alerts or yellow alerts, depending on the data that’s coming. At the backend we can see those people that we need to contact immediately. And there are fail safes in that system as well. If the patient isn’t alerted, if that patient isn’t contacted and an action taken within a certain timeframe, then that generates an alert as well.
The important concept is that we’re promptly attending to those with the greatest need, and monitoring potentially large amounts of people with a small number of staff members.
Being cloud–based also means that if necessary those staff members can also access the system remotely – for example if they have been quarantined, but still feel well enough, they can work from home and still provide patient support via the platform.
In general, the system will be used to monitor COVID-19 positive patients for 10-14 days, or until their doctor is satisfied that they are out of danger and no longer an infection risk.
Future plans
At present the COVID-19 monitoring system is triggered by the patient’s data and clinician set thresholds for that data, but in the future there are opportunities to leverage a range of Azure cognitive services.
The COVID and cardiac monitoring systems are just two in a series of telehealth solutions that are envisaged to play critical roles in SESLHD’s Virtual Care Centre which is in the process if being developed between now and 2022 as the POWH Acute Services Building is commissioned but the global pandemic has now fast-tracked our service.
Clinicians hope that by forging links between various monitoring systems it is possible to get a multiplier effect to improve the outcomes for patients.
Ooi explains; “Our focus is shifting to elderly cardiac patients and elderly respiratory patients in the community who are vulnerable and at–risk if they do contract COVID, and finding a solution for their remote monitoring in the community.” That will relieve the burden from the community heart failure team and also reduce the risk to them and their patients of close physical contact while COVID-19 remains a significant risk.
“We are in a position to deploy the cardiac solution on the back of the COVID solution and immediately recruit patients across SESLHD and other local health districts – enrolling community heart failure patients so that we can be monitoring them safely at home.”
Because of the need to take rapid action on COVID monitoring Ooi says that the organisation has fast tracked to where it thought it might have been three to five years from now, in its bid to offer a remote monitoring solution for patients across multiple medical and surgical disciplines.
“The dream is to create a modular app with a singular backend that’s staffed by the POWH Remote Monitoring Solution in the Virtual Care Centre. Clinicians can prescribe an app for their patient to support their treatment, they can go to an IT hub to get it uploaded, they get trained, they get provided with the appropriate peripherals, whatever they are, because there are so many different biosensors. The app then provides the patient with support, education and monitoring of important physiological data as they transition from acute hospital care back into the community.”
If there is a silver lining to COVID-19 he says it is that it has proven healthcare can be delivered in new ways that are just as effective, secure and private.
Lovell agrees; “I think that this has created a huge sea change. What we’ve really tried to focus on, both with COVID and the TeleClinical Care – Cardiac solution is co-designing with clinicians and understanding how it works for patients and incorporating patient and consumer feedback in a co-design process.”
We’re focused on supporting our customers during these difficult times. For more information on how we can help your business, please see our dedicated webpage and report on Supporting Resilient Operations. We’ll be updating these resources regularly as the situation evolves.